Simple management protocol for Closed Nasal Reduction (broken nose surgery procedure)
- Doctor CO
- May 22, 2018
- 4 min read
Performing the initial physical examination and history is a critical step. Posttraumatic edema, preexisting nasal deformity, or a discrete septal fracture may complicate the physical examination and may lead to unrecognized acute deformity.
First, external evaluation to determine nasal deviation followed by an internal examination with proper lighting and a nasal speculum should be performed on all patients who present to the emergency room or clinic. On physical examination, it is important to palpate the nasal bones to identify areas of collapse and/or asymmetry. Tenderness on palpation may help to elucidate the age of a fracture, as patients may present with new fractures following a history of old nasal deformity. Presence of septal hematoma, deviation, and mucosal disruption should be recorded. A septal hematoma is considered an emergent issue and should be drained immediately on identification in the emergency room or clinic setting.
Second, often overlooked, it is important to evaluate the relationship of the upper lateral cartilages of the nose to the nasal bones, referred to as the keystone region.

The presence of an avulsion of cartilage from the nasal bones is a critical finding on physical examination that affects management. If this exists, closed reduction of the nasal bones alone will not be sufficient to treat the acquired nasal deformity, commonly resulting in a unilateral collapse of the nasal sidewall. On physical examination, it may appear as significant concavity and “hollowed-out” appearance on the avulsed side.

Functionally, this injury may impede the nasal airway by encroachment and collapse of the internal nasal valve, particularly during inspiration.

These avulsion injuries require suturing of the upper lateral cartilages back to the nasal bone to maintain reduction. Internal nasal packing alone is typically inadequate to treat upper lateral cartilage avulsion.

Third, in preparation for closed reduction, pledgets soaked in oxymetazoline(Afrin) are placed intranasally. Oxymetazoline is a selective alpha-1 agonist resulting in vasoconstriction. We find this useful for reducing the amount of bleeding from mucosal damage incurred on manipulation, but it is not mandatory. Three soaked pledgets are placed in each nostril with bayonet forceps: one adjacent to the septum, one above the inferior turbinate, and one below the turbinate. Although exceptionally rare, cardiac instability and hypertension have been reported with the use of Afrin-soaked pledgets.
Fourth, after waiting 5-10 minutes for the vasoconstrictive effects of the oxymetazoline, manipulation of the fracture can be performed with abated bleeding. Using a Boies elevator, reduction is initiated. An important step to take before insertion of the Boies elevator is to measure the length from the caudal edge of the alar rim to the nasofrontal suture. This ensures that the Boies elevator does not damage the cribriform plate. The thumb and index finger are then placed on the nasal bridge.
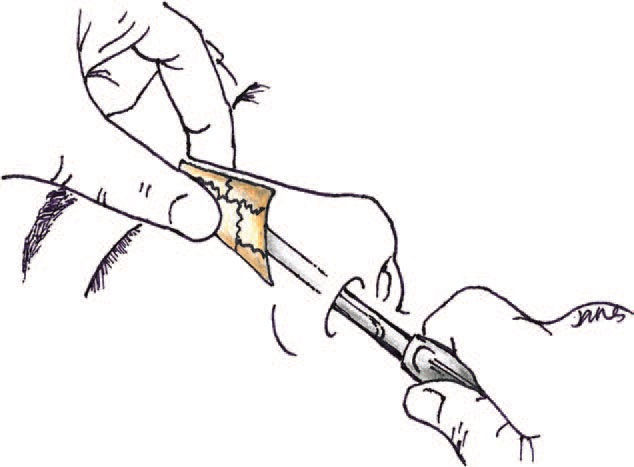
Once inserted and sitting under the nasal bone, the Boies elevator is pulled in an anterior (forward) direction to straighten the nose and bring a deviated nasal dorsum back to the midline.

This is repeated on the opposite side. Because of comminution, which is typical of nasal bones, a “pop” should not be anticipated. During this time, the Boies elevator can also be guided into the nasopharynx to ensure that there is no concomitant airway obstruction caused by a deviated septum.
Fifth, using the Boies elevator, the vertically oriented instrument (placed adjacent to the septum) is then rotated and canted out laterally to allow for reduction of any collapsed bony segments.

Depending on the degree of comminution, the surgeon must anticipate the possibility that the bony segments may recollapse even after initial reduction, necessitating support with nasal packing.
Sixth, if there is a septal injury, reduction is achieved by using Asch septum straightening forceps. They are placed with one tine in each naris. The instrument is then closed sequentially in an inferior to superior direction to straighten any septal deformity.

Doyle Open Lumen Septal Splints (Doyle Medical Devices, Stockton, Calif.) are then placed and secured with a trans-septal (horizontal mattress) permanent suture. We prefer to pass the suture through the membranous portion of the inferior septum, avoiding the columella, to prevent tissue necrosis and reduce patient discomfort.
Seventh, once adequate reduction and symmetry is achieved by these simple maneuvers, half-inch-wide petroleum jelly (Vaseline)–impregnated gauze is packed directly underneath the nasal bones on both sides.

This will prevent collapse of the reduced segments and may have the opposite effect, bowing the nose outward because of the initial unopposed outward pressure placed on the nose with this technique. There is currently no clear data on how long packings can safely stay in place. However, our practice is to instruct patients to remove the nasal packings after 72 hours to minimize the possibility of toxic shock syndrome. For the duration of nasal packing, we place the patient on prophylactic antibiotics. We have not experienced any complications from nasal packing for this duration.
Finally, liquid adhesive is placed over the nasal bridge and nose extending slightly onto the cheek. Steri-Strips are then cut to size and placed over the adhesive application area. An aluminum Denver Splint is placed on the nasal bridge with pressure applied laterally to provide external compression of the reduced segments against the internal packing.

This maneuver provides an opposing force to the internal petroleum gauze packings, stabilizing the bones between these two structures. Denver Splint is preferred to Aquaplast nasal splints because the aluminum is sturdier, maintaining a more reliable triangular shape. Steri-Strips are then applied over the splint to provide additional support. A temporary mustache dressing is placed underneath the nostrils on completion of the procedure to collect any residual drainage.

Designed with priorities of patient well-being and accommodation. Doctor recommended, patented design offers a solution to a common and plaguing dilemma. Doctor CO Eyewear® is a vital innovation that enables users to wear glasses following facial surgeries while eliminating pressure, creases or dents in the nasal tissues and the risk of additional expensive surgeries.
Protect your expensive rhinoplasty investment with a remarkably simple solution. Doctor CO Eyewear® will easily and quickly allow you to resume wearing glasses while providing critical protection and get back to the life style you enjoy.
![[꾸미기]doctor+co+eyewear+원본+고해상도_대지+1 (1).jpg](https://static.wixstatic.com/media/d7dab4_76e9c7054fc648e79721c25d4505c68f~mv2.jpg/v1/fill/w_255,h_57,al_c,q_80,usm_0.66_1.00_0.01,enc_avif,quality_auto/%5B%EA%BE%B8%EB%AF%B8%EA%B8%B0%5Ddoctor%2Bco%2Beyewear%2B%EC%9B%90%EB%B3%B8%2B%EA%B3%A0%ED%95%B4%EC%83%81%EB%8F%84_%EB%8C%80%EC%A7%80%2B1%20(1).jpg)







Comments